Abstract
Objectives
We evaluated clinical characteristics including adherence and its effects on overall survival (OS) in Korean patients diagnosed with chronic myeloid leukemia (CML) using National Health Information Database "NHID".
Methods
This study included patients 15 and older who were diagnosed with Philadelphia chromosome positive CML (ICD code C921) from 2005 to 2013 and prescribed with tyrosine kinase inhibitors (TKIs). TKIs included imatinib, dasatinib, nilotinib and radotinib which were covered by the National Health Insurance Service (NHIS) currently.Patients who were received interferon, prescribed TKI only once, or prescribed TKI 6 months after diagnosis were excluded. We extracted age, sex, medical institution, medical insurance premium (which is imposed by proportionate to income), medication list, date of hematopoietic stem cell transplantation (HSCT), and date of death from NHID. Each patients' laboratory result or disease phase (chronic phase, accelerate phase, or blastic crisis) were not available. Medication possession ratio (MPR) was used for adherence. Overall Survival (OS) was calculated by Kaplan-Meier methods. As well as, univariate and multivariate analysis were done with Cox proportional hazard regression using SAS with following variables: Sex, age (≤50 years vs 50> years), income (high (upper 50%), low (lower 50%)), frontline TKI (imatinib vs others), and adherence (high (MPR ≥0.90), low (MPR<0.9)).
Results
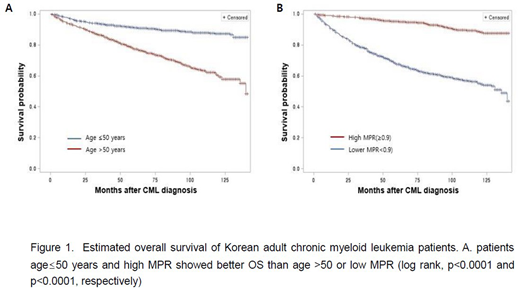
A total of 3146 were followed up with a median of 69 (1-147) months until the end of 2016. Male was 60.2% (n=1899). Median age was 50 (16-92). More patients (n=1991, 62.9%) payed higher insurance premium. Imatinib was most frequently prescribed TKI (n=2764, 87.4%), then dasatinib (n=904, 28.6%), nilotinib (n=760, 24.0%), and radotinib (n=145, 4.6%) followed in orders. About two-thirds (n=2055, 65%) maintained frontline TKI until the end of follow up. Imatinib was selected as frontline TKI in 86.2% (n=3310), and 13.8% of patients chose newer generation TKIs. After TKI treatment, 7.7% of the patients received cytotoxic chemotherapy, and 19 patients underwent HSCT. Median MPR was 0.975 (0.003-2.035). A total 62% of patients (n=1966) showed high adherence. Male (p=0.036), young age (p<0.0001), high income (p=0.0002), using newer generation TKIs in the frontline (p<0.0001), and longer TKI treatment duration (p<0.0001) were associated with better adherence. Patients with low MPR performed chemotherapy (p<0.0001) or HSCT(p<0.0001) and expired (p<0.001) more than those with high MPR. Estimated OS at 5-year and 10-year were 84.7% and 75.3%, respectively. In univariate analysis, patients older than 50-years (HR 2.11 [95% C.I. 1.81-2.47] (Figure 1A) and low MPR (HR 6.34[95% CI 5.22-7.70] (Figure 1B) showed poor OS. In multivariate analysis, male, age >50, low MPR patients associated with poor OS showing HR 1.29 [95% C.I., 1.09-1.52], 2.98 [95% C.I., 2.49-3.58], and 6.13 [95% C.I., 5.04-7.45], respectively.
Conclusion
Based on NHID, estimated OS of 3146 Korean CML patients at 10-year was 75.3%, and female, age ≤50, and high MPR associated with better OS.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal